Lowering prescription drug prices has been a priority for President Donald Trump since taking office in January. He has taken a number of steps, including striking deals with drug companies to lower the cost of prescription drugs.
President Trump also directed the Food and Drug Administration (FDA) to streamline its regulatory process to facilitate the availability of cheaper, counterfeit drugs such as generic drugs and biosimilars.
Recommended stories
list of 3 itemsend of list
Biosimilars are very similar versions of biologics, a group of medicines that are manufactured through biological processes. One of the most widely used biologics is insulin, which is used to treat diabetes.
BIologics, which account for just 5% of prescriptions, account for more than half of total spending on drugs in the U.S., according to health data analytics firm IQVIA.
The Trump administration has said it wants to make these drugs more affordable by increasing access to biosimilars.
So what are biologics and biosimilars, and can the government’s proposals help reduce their use? cost?
What is a biological product?
Biologic is an abbreviation for biological drug or product. This is a broad category of products including vaccines, blood and blood components, gene therapy and tissues. These are a type of complex drugs that are produced through biological processes or from living organisms such as proteins and genes. They treat cancer, autoimmune diseases, and other rare diseases.
Biologics are typically administered by injection or infusion, said Alex Keaton, executive director of the Association for Accessible Medicine’s Biosimilars Council, an industry group that advocates on behalf of biosimilar manufacturers.
The FDA’s approval process for these products is rigorous and typically takes 10 to 15 years, said Brian Chen, a health law and economics expert at the University of South Carolina. In unusual circumstances, faster scheduling is possible. For example, federal agencies work with vaccine manufacturers and scientists to accelerate the development of COVID-19 vaccines.
What is a biosimilar?
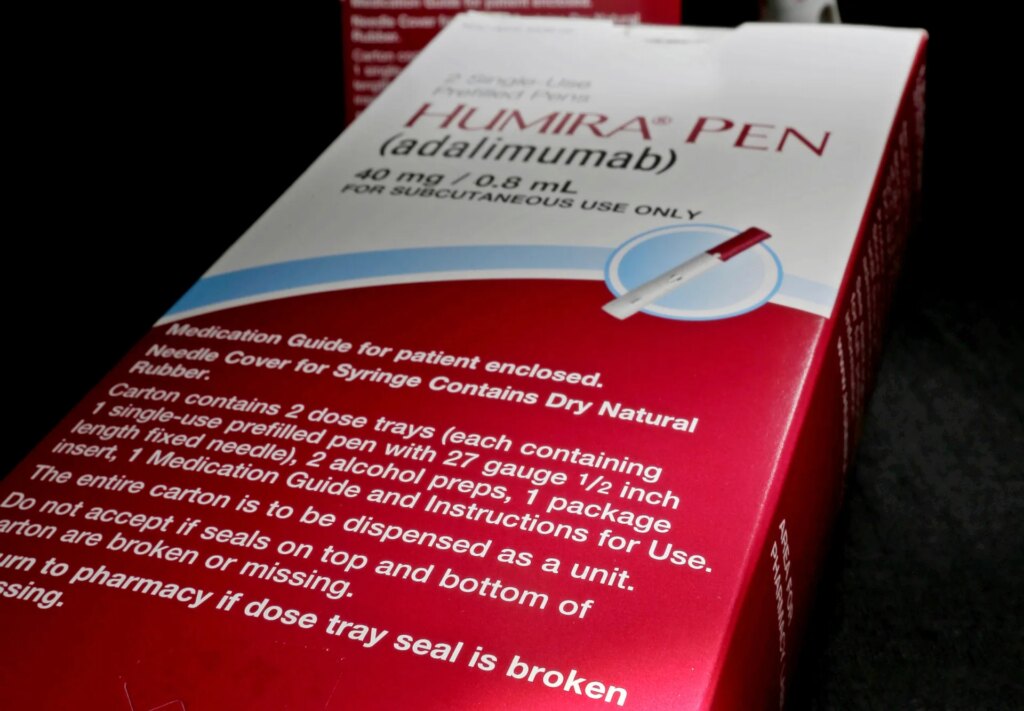
As the name suggests, these drugs are similar to the original biologics approved by the FDA. Keaton said biosimilars are developed and marketed after the original biologic loses patent exclusivity. Humira biosimilars used by rheumatoid arthritis patients include Siltezo, Amjevita, and Idacio.
“They work the same clinically, but they’re not exactly the same,” Keaton says.
That’s because, unlike brand-name generic drugs, it’s impossible to make an exact copy of a biologic drug. Biologics have complex manufacturing processes and their ingredients are derived from living organisms.
“Biologics are like flexible strands of cooked spaghetti that are folded in a very specific way, making exact replication nearly impossible,” Chen said.
FDA evaluates proposed biosimilar products against the original biological product to determine whether the products are very similar and have no clinically significant differences. It is expected to have the same benefits and risks as the original biologic. To be approved, biosimilar manufacturers must demonstrate that patients using their product have no new or worsening side effects compared to patients using the original biologic.
Keaton said FDA approval of biosimilars often takes five to six years.
Biosimilars increase market competition and encourage brand-name drug manufacturers to lower prices.
How much do biologics and biosimilars typically cost?
They are expensive and the exact cost varies.
One 2018 study found that the use of biologics and biosimilars can cost U.S. patients an average of $10,000 to $30,000 per year.
Humira is more. It was listed in early November for $6,922 per month. Siltezo, a biosimilar to Humira, is advertising a 5% discount on the price of Humira. The makers of Cyltezo also offer a non-brand name option at a price of $550 for those who pay cash at the pharmacy while using the GoodRx app.
The actual amount an insured person pays also depends on the rate negotiated by the plan and insurance company.
One 2024 study found that prices for biosimilars are typically 15-35% lower than brand-name biologics. The FDA found that biologics offer more dramatic cost savings, averaging 50%.
Why are these drugs so expensive?
Biologics and biosimilars are difficult and expensive to develop and produce.
It takes five ingredients to make a standard over-the-counter drug, such as aspirin. Genetic modification of living organisms is required to produce insulin, a biological drug.
These complex manufacturing procedures and proprietary information make it difficult for competitors to create substitutes.
To put this into perspective, as of July, there were 226 biologics on the market in the United States, and the FDA had approved 76 biosimilars, including insulin. When it comes to non-biological drugs, the FDA has approved over 32,000 generic drugs. This is more than the number of brand-name drugs approved.
Can a biosimilar be used in place of the original FDA-approved biologic?
yes. All biosimilars must meet FDA requirements and must be highly similar and not clinically meaningfully different from existing FDA-approved biosimilars.
So how does the Trump administration want to change the FDA’s biosimilar approval process?
Under the draft guidance, the government proposed reducing some of the testing required as part of the FDA process used to prove that biosimilar drugs are as safe and effective as biological drugs.
Currently, manufacturers requesting biosimilar licenses must provide clinical research data demonstrating the similarity of their products. The FDA’s new proposal would no longer require drug developers to conduct such comparative clinical trials.
Manufacturers will still need to test proposed biosimilars. Other data, such as comparative analyzes showing how the drug moves through the body, immune response data, and human study data, may be sufficient to demonstrate that the drug is similar to existing biologics, the FDA said.
Why would the FDA want to change the biosimilar approval process?
Keaton said the agency ultimately aims to encourage drug companies to develop biosimilars quickly by eliminating redundant, costly and time-consuming clinical studies.
Saving that time could increase the number of biosimilar alternatives.
This will almost certainly reduce front-end development costs for pharmaceutical companies, Chen said.
Will that change lower the cost of the drugs for patients who need them?
Regulatory changes alone may not significantly lower prices for many Americans.
A report from the U.S. Department of Health and Human Services says some off-brand options need to be made available to significantly lower prices.
However, even with more options, the price may remain the same.
A 2024 study published in the health policy journal JAMA Health Forum found that annual out-of-pocket costs for most biologics increased or remained stable even after biosimilars became available. Patients who took the biosimilar did not pay less than patients who took the original biologic.
That’s at least in part because biologics manufacturers often offer large rebates to pharmacy benefit managers, companies that work with insurers, employers and others to manage prescription drug plan benefits. In return, insurers would give the branded biologics preferential or exclusive coverage on their list of covered drugs, Chen said. The rebate wall will ultimately hinder the sale of cheaper biosimilars, he said.
Are there other obstacles to bringing more biosimilars to market?
Yes, one more important hurdle remains. Manufacturers of name-brand biologics hold many patents and often file lawsuits to block the commercial sale of approved biosimilars.
A 2018 study conducted by Chen found that of the 12 biosimilar products approved by the FDA, five were commercially available as of October 2018. The remaining six items were not available due to patent disputes.
PolitiFact researcher Caryn Baird contributed to this report.